Resumen
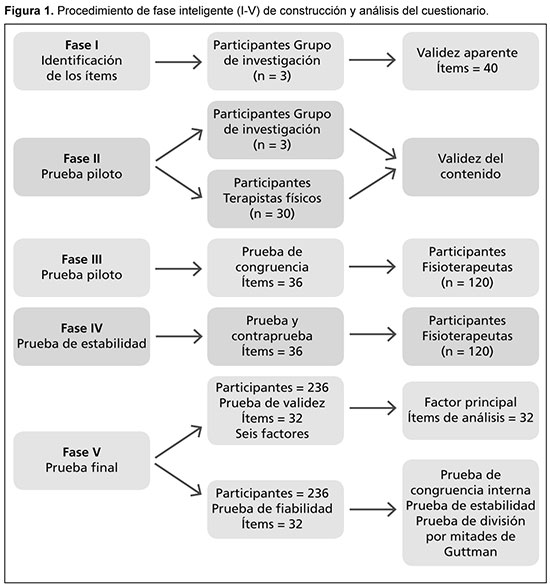
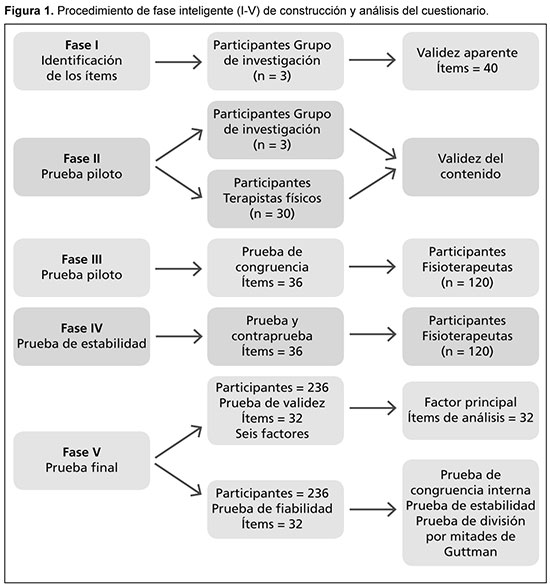
Introducción: El dolor lumbar (DL) constituye un problema de salud considerable en muchos países y, en ocasiones, puede persistir por más de 12 semanas. Es la causa más común de discapacidad funcional que afecta al grupo de adultos, con una tasa de prevalencia del 84%. Propósito: Se carece a nivel mundial de un análisis de rendimiento confiable y válido, orientado a objetivos que utilice una escala de Likert para evaluar el grado de satisfacción del fisioterapeuta en el tratamiento de sujetos con DL. Por lo tanto, se elabora y valida un cuestionario utilizado para tal fin. Sujetos y métodos: En la primera fase, los elementos del cuestionario inicial se seleccionaron según los signos y síntomas del DL. En la segunda fase, se analizó la validez hacia los del contenido mediante el envío del cuestionario revisado a 30 fisioterapeutas para sus comentarios. En la tercera y cuarta fases, el cuestionario revisado final se envió a 120 fisioterapeutas, que ejercían su práctica profesional, para verificar la congruencia de los ítems. En la quinta fase, se midieron la validez final (análisis factorial) y la confiabilidad (congruencia interna) del cuestionario. Resultados: El cuestionario final consta de 32 ítems con seis factores. La confiabilidad (coeficientes alfa de Cronbach) para los ítems varió de 0.67 a 0.85 y la estabilidad (coeficiente de división por mitades de Guttman) para la prueba y contraprueba varió entre 0.68 a 0.89. Se realizó una prueba de validez mediante un análisis factorial principal con un puntaje de corte de 0.6. Conclusión: El cuestionario de satisfacción del fisioterapeuta fue confiable y válido para determinar su grado de satisfacción en el tratamiento de sujetos con DL.
Resumen
Introducción: El dolor lumbar (DL) constituye un problema de salud considerable en muchos países y, en ocasiones, puede persistir por más de 12 semanas. Es la causa más común de discapacidad funcional que afecta al grupo de adultos, con una tasa de prevalencia del 84%. Propósito: Se carece a nivel mundial de un análisis de rendimiento confiable y válido, orientado a objetivos que utilice una escala de Likert para evaluar el grado de satisfacción del fisioterapeuta en el tratamiento de sujetos con DL. Por lo tanto, se elabora y valida un cuestionario utilizado para tal fin. Sujetos y métodos: En la primera fase, los elementos del cuestionario inicial se seleccionaron según los signos y síntomas del DL. En la segunda fase, se analizó la validez hacia los del contenido mediante el envío del cuestionario revisado a 30 fisioterapeutas para sus comentarios. En la tercera y cuarta fases, el cuestionario revisado final se envió a 120 fisioterapeutas, que ejercían su práctica profesional, para verificar la congruencia de los ítems. En la quinta fase, se midieron la validez final (análisis factorial) y la confiabilidad (congruencia interna) del cuestionario. Resultados: El cuestionario final consta de 32 ítems con seis factores. La confiabilidad (coeficientes alfa de Cronbach) para los ítems varió de 0.67 a 0.85 y la estabilidad (coeficiente de división por mitades de Guttman) para la prueba y contraprueba varió entre 0.68 a 0.89. Se realizó una prueba de validez mediante un análisis factorial principal con un puntaje de corte de 0.6. Conclusión: El cuestionario de satisfacción del fisioterapeuta fue confiable y válido para determinar su grado de satisfacción en el tratamiento de sujetos con DL.
 Palabras clave
dolor lumbar, cuestionario dolor lumbar
Palabras clave
dolor lumbar, cuestionario dolor lumbar
 Abstract
Abstract
Introduction: Low back pain (LBP) is a considerable health problem in many countries and may sometimes last for more than 12 weeks. It is the most common cause of functional disability affecting the adult group with a prevalence rate of 84%. Purpose: A reliable and valid goal-oriented performance analysis using a Likert scale for therapist´s satisfaction in treating subjects with low back pain (LBP) has been lacking globally. Therefore, a questionnaire used for therapist´s satisfaction in treating low back pain (LBP) is developed and validated. Subjects and methods: In the first phase, the items in the initial questionnaire were selected as per the signs and symptoms of low back pain (LBP). In the second phase, the content validity was analyzed by sending the revised questionnaire to 30 physical therapists for their comments. In the third and fourth phases, the final revised questionnaire was sent to 120 practicing therapists for checking the consistency of the items. In the fifth phase, the final validity (factor analysis) and reliability (internal consistency) of the questionnaire were measured. Results: The final questionnaire consists of 32 items with six factors. The reliability (Cronbach's alpha coefficients) for items ranged from 0.67 to 0.85 and the stability (Guttman split-half coefficient) for test-retest ranged from 0.68 to 0.89. A validity test was done by a principle factor analysis with a cut-off score of 0.6. Conclusion: The physiotherapist satisfaction questionnaire was reliable and valid for finding the physiotherapist´s satisfaction in subjects with low back pain.
 Key words
Key words
questionnaire low back pain, Likert scale
Artículo completo
TRATAMIENTO DEL DOLOR LUMBAR: CUESTIONARIO SOBRE LA SATISFACCION DE LOS FISIOTERAPEUTAS
(especial para SIIC © Derechos reservados)
Introducción
El dolor lumbar (DL) constituye un problema de salud considerable en muchos países, y en ocasiones, puede persistir por más de 12 semanas.1 Es la causa más común de discapacidad funcional que afecta al grupo de adultos, con una tasa de prevalencia del 84%.2 Contribuyen a esta condición la salud general, el nivel socioeconómico y los factores ambientales.3 Tiene un efecto significativo en las actividades ocupacionales y es una causa importante de enfermedad y ausentismo laboral.4,5
El enfoque de la lumbalgia constituye un desafío y requiere una evaluación clínica compleja. Durante el proceso de evaluación, los fisioterapeutas solían considerar la información subjetiva, los antecedentes de dolor, el examen físico, el estado mental y la calidad de vida.6,7 La información subjetiva comprende los antecedentes de salud, así como personales, psicológicos y sociales.8 La terapia física para el DL tiene varias modalidades de ejercicios físicos y terapéuticos que pueden influir en el grado de satisfacción.9
Investigaciones recientes sobre el DL demuestran que los pacientes sintieron un alto grado de dolor, discapacidad, trastornos en las actividades regulares y problemas psicosociales como ansiedad y depresión. Estos factores pueden influir en la satisfacción con la atención médica.10,13 Como fisioterapeuta, es importante tener una comprensión profunda del paciente para planificar un tratamiento eficaz.14 Los fisioterapeutas deben escuchar atentamente los antecedentes del paciente y observar los signos y síntomas físicos, para lo cual se requiere capacitación y habilidades adecuadas.15,16 Para lograr una satisfacción completa en el desempeño orientado a objetivos, se requiere una evaluación minuciosa del paciente.17
Cada vez más se utilizan cuestionarios de satisfacción del paciente para monitorear sus percepciones18 y se dispone de otros cuestionarios para medir la satisfacción con las internaciones, las visitas al consultorio médico y el seguro de salud.19,20 Sin embargo, se carece a nivel mundial de un análisis de desempeño orientado a objetivos válido y confiable que utilice la escala de Likert para determinar el grado de satisfacción del fisioterapeuta en el tratamiento del DL, por lo tanto, se planificó esta investigación. El estudio se realizó con el objetivo de elaborar un cuestionario para medir el rendimiento orientado a objetivos con una escala de Likert para determinar la satisfacción del fisioterapeuta en el tratamiento de las personas con DL.
Pacientes y métodos
La elaboración de un cuestionario para la evaluación de la satisfacción del fisioterapeuta en el tratamiento de los pacientes con DL requirió diversos procedimientos. Los ítems del cuestionario se basaron en los comentarios de los fisioterapeutas y los pacientes, así como en los informes de investigación de la bibliografía más reciente. Su diseño se basó principalmente en los signos y síntomas clínicos del DL.
El estudio se realizó en seis ciudades metropolitanas de la India y la población de estudio comprendió a fisioterapeutas que trabajan en hospitales universitarios, gubernamentales y privados y en clínicas privadas. Se utilizó un diseño de muestra aleatorizada, estratificada por conglomerados y se definieron cuatro estratos según el área de trabajo. Se seleccionó al azar un número igual de participantes de los cuatro estratos.
Para ser elegible para su inclusión en el estudio, los profesionales debían haber completado al menos su programa de grado de cuatro años y debían estar trabajando en el ámbito clínico sin ninguna limitación en su práctica. Los participantes fueron excluidos si tenían otros títulos de grado o si trabajaban en centros académicos y como personal profesional de otros centros médicos.
En la primera fase, se seleccionaron los ítems de la bibliografía más reciente mediante el uso de palabras clave en las bases de datos y se confirmaron los que fueron apropiados, claros y relevantes. El grupo de investigación multidisciplinario (GIM) analizó la validez aparente de los ítems por medio de diferentes aspectos. En la segunda fase, se analizó la validez del contenido mediante el envío del cuestionario revisado a los fisioterapeutas (primer piloto) para sus comentarios. Los ítems se modificaron según los comentarios de los fisioterapeutas y el cuestionario revisado se les envió nuevamente (segunda prueba piloto) para concluir los ítems.
En la tercera fase, el cuestionario final revisado se envió nuevamente a los fisioterapeutas en ejercicio profesional (tercer piloto) para verificar la congruencia de los ítems. En la cuarta fase, se realizaron modificaciones menores según los resultados de congruencia interna y se enviaron a los fisioterapeutas para analizar la estabilidad de los ítems. En la quinta fase, se midió la validez final (análisis factorial) y la confiabilidad (congruencia interna) del cuestionario (Figura 1).
El estudio recibió la aprobación ética del comité de ética institucional (Ref: CUSPC/ética/146-A/09) y cumplió con la Declaración de Helsinki. Se obtuvo el consentimiento por escrito de los sujetos que indicaban que la participación fue voluntaria y también se obtuvo el permiso para realizar el estudio en los hospitales y clínicas. Se distribuyó información detallada sobre el estudio y el cuestionario a todos los sujetos. Se mantuvo la confidencialidad de los datos personales de los participantes, al igual que el enmascaramiento del cuestionario.
Se pidió a los sujetos que completaran el cuestionario y lo enviaran de regreso en un sobre con la dirección del remitente. Los datos recopilados se mantuvieron confidenciales y por un miembro en cada región. Las opciones de respuesta para los ítems se calificaron en una escala de diez puntos, que van de “negativo” a “positivo”. Cada ítem midió un aspecto diferente de DL y se calificó por separado. A mayor puntaje, mayor el grado de satisfacción del fisioterapeuta.
La fiabilidad del cuestionario se analizó mediante la prueba de congruencia interna (coeficiente alfa de Cronbach)21,22 y la prueba de estabilidad (coeficiente de división por mitades de Guttman).23 La validez de constructo del cuestionario se realizó mediante el método de análisis factorial por medio de la identificación de los ítems en cada factor.24 La posibilidad de extraer factores se examinó con la prueba de Kaiser-Meyer-Olkin (KMO) y el puntaje cercano a 1 se consideró como bueno y el de 0.6 como aceptable. Los puntajes inferiores a 0.6 en el análisis KMO no se consideraron adecuados y se eliminaron del análisis. El análisis se realizó mediante el software SPSS para Windows, versión 18.0, Chicago: SPSS Inc.
Resultados
Selección de artículos: validez aparente
En primer lugar, se realizó un análisis crítico de la bibliografía sobre los signos y síntomas clínicos de sujetos con DL para seleccionar los ítems. Las bases de datos como Pubmed, CINHAL, Medline, Embase y Google Scholar se usaron para identificar los artículos y también se utilizaron para tal fin las palabras clave. Se formó un grupo de investigación multidisciplinario (GIM) que consistió en un cirujano ortopédico, un fisioterapeuta y un trabajador social para monitorear todo el proceso. El primer borrador consistió en 40 ítems, que se presentaron al GIM para su análisis inicial y sugerencias. El grupo sugirió el uso de frases simples, directas y cortas para comprender los ítems por todo tipo de profesionales médicos. Los artículos se revisaron según los comentarios del equipo de investigación.
Estudios piloto: validez de contenido
El cuestionario revisado se envió a 30 fisioterapeutas (primer piloto) y se les dieron instrucciones para completar los ítems del cuestionario. Entre ellos, tres se negaron a completarlo; tres argumentaron que los ítems presentados fueron demasiado difíciles para asignarles un puntaje y dos declararon que no tenían tiempo para completarlos. Alrededor de 22 evaluaron los ítems y algunos comentaron que eran demasiado difíciles de examinar y difíciles de calificar. Algunos informaron que los ítems a ser examinados y calificados llevaban demasiado tiempo. Según los comentarios recibidos, el investigador hizo el cuestionario corto y simple de comprender y para ser completado rápidamente. Los ítems del cuestionario se subcategorizaron nuevamente según la sugerencia del grupo de investigación y se muestran a continuación:
1. Dolor y movimiento articular.
2. Función muscular.
3. Sensación y equilibrio.
4. Habilidad funcional.
5. Estado mental.
6. Calidad de vida.
El cuestionario revisado se envió nuevamente a 24 fisioterapeutas (segunda prueba piloto) para identificar la viabilidad de aplicación. Según los comentarios de los terapeutas, se eliminaron cuatro ítems y los ítems del cuestionario se redujeron a 36.
Congruencia de artículos
El cuestionario revisado final junto con la carta informativa, las instrucciones para completar el cuestionario y el sobre con la dirección del remitente se enviaron a 120 fisioterapeutas (tercer prueba piloto). Entre ellos, 96 (80%) completaron y devolvieron los cuestionarios con comentarios positivos. Los resultados del estudio mostraron una buena congruencia interna con un rango alfa de Cronbach de 0.68 a 0.87 para todas las subescalas y con otros ítems en el cuestionario.
Estabilidad de los ítems
Se realizó una nueva prueba para evaluar la fiabilidad después de realizar cambios menores en el cuestionario en función de los resultados de los análisis de congruencia interna. El cuestionario se envió nuevamente a los 120 terapeutas para evaluación de seguimiento y estabilidad. Los coeficientes alfa de Cronbach para las subescalas variaron entre 0.67 y 0.85. Los ítems con el coeficiente de división por mitades de Guttman para prueba y contraprueba que oscilaron entre 0.68 a 0.89 se retuvieron en el cuestionario. Cuatro ítems con bajos coeficientes de correlación (0.32, 0.38, 0.41 y 0.45) se excluyeron del cuestionario y los ítems se redujeron a 32.
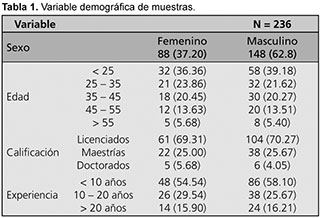
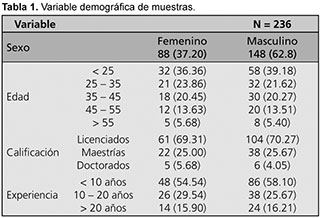
Prueba final de validez y confiabilidad: se analizaron los ítems finales revisados y modificados en el cuestionario para determinar su validez y confiabilidad. Un total de 236 (80.82%) fisioterapeutas de 292 participaron en el estudio, con 37.2% hombres y 62.8% mujeres. El 70% eran licenciados, el 25% tenía una maestría y el 5% un doctorado; los fisioterapeutas con menos de 10 años de experiencia fueron 57%, con 10 a 20 años de experiencia fueron 27% y con más de 10 años de experiencia fueron 16% (Tabla 1). Se realizó una prueba de validez por análisis factorial principal para todos los ítems del cuestionario. Quedaron 32 ítems para el análisis factorial final después del análisis KMO con una puntuación de corte de 0.6 (Tabla 2). El puntaje de KMO fue de 0.86 para todos los ítems en 6 factores y la prueba de esfericidad de Barlett fue significativa (p < 0.001).

Factor uno. Dolor y movimiento articular. El primer factor tiene seis ítems y los resultados muestran que los seis ítems en el factor uno enuncian un componente porque el coeficiente de correlación entre ítems en el factor uno fue positivo y significativo, con un valor de p < 0.001 (Tabla 3). El porcentaje total de la varianza de este factor fue del 17.68%. La prueba de confiabilidad se analizó con congruencia interna y probada por el alfa de Cronbach, que fue de 0.84 para los seis ítems en el factor uno. La estabilidad de la prueba y contraprueba se realizó mediante el coeficiente de división por mitades de Guttman, que fue de 0.78 y que muestra la alta estabilidad de los ítems.

Factor dos. Función muscular. El segundo factor tiene seis ítems y los resultados muestran que los seis ítems en el factor dos enuncian un componente porque el coeficiente de correlación entre ítems en el factor dos fue positivo y significativo, con unvalor de p < 0.001 (Tabla 3). El porcentaje total de la varianza de este factor es 18.21%. El coeficiente alfa de Cronbach fue de 0.78 y el coeficiente de división por mitades de Guttman fue de 0.72, lo que sugiere fiabilidad y estabilidad de los ítems.
Factor tres. Sensación y equilibrio: el tercer factor tiene cinco ítems y los resultados muestran que los cinco ítems en el factor tres enuncian un componente porque el coeficiente de correlación entre ítems en el factor tres fue positivo y significativo, con un valor de p < 0.001 (Tabla 3). El porcentaje total de la varianza de este factor es 12.81%. El coeficiente alfa de Cronbach fue de 0.78 y el coeficiente de división por mitades de Guttman fue de 0.82, lo que sugiere fiabilidad y estabilidad de los ítems.
Factor cuatro. Capacidad funcional: el cuarto factor tiene seis ítems y los resultados muestran que los seis ítems en el factor cuatro enuncian un componente porque el coeficiente de correlación entre ítems en el factor cuatro fue positivo y significativo, con una p < 0.001 (Tabla 3). El porcentaje total de la varianza de este factor es 17.67%. El coeficiente alfa de Cronbach fue de 0.78 y el coeficiente de división por mitades de Guttman fue de 0.69, lo que sugiere fiabilidad y estabilidad de los ítems.
Factor cinco. Estado mental: el quinto factor tiene cinco ítems y los resultados muestran que los cinco ítems en el factor cinco enuncian un componente porque el coeficiente de correlación entre ítems en el factor cinco fue positivo y significativo, con una p < 0.001 (Tabla 3). El porcentaje total de la varianza de este factor es 13.12%. El coeficiente alfa de Cronbach fue de 0.78 y el coeficiente de división por mitades de Guttman fue de 0.71, lo que sugiere fiabilidad y estabilidad de los ítems.
Factor seis. Calidad de vida: el sexto factor tiene cuatro ítems y los resultados muestran que los cuatro ítems en el factor seis enuncian un componente porque el coeficiente de correlación entre ítems en el factor seis fue positivo y significativo, con un valor de p < 0.001 (Tabla 3). El porcentaje total de la varianza de este factor es 8.21%. El coeficiente alfa de Cronbach fue de 0.78 y el coeficiente de división por mitades de Guttman fue de 0.77, lo que sugiere fiabilidad y estabilidad de los ítems.
El cuestionario final. El cuestionario final (Apéndice A) consistió en 32 ítems en seis factores. El primer factor comprendió seis ítems que evaluaron el estado del dolor y el movimiento articular. El segundo factor que contenía seis ítems evaluó la función muscular. El tercer factor, evaluó la sensación y el equilibrio, contenía cinco ítems. El cuarto factor, con seis ítems, evaluó la capacidad funcional. El quinto factor con cinco ítems evaluó el estado mental y el factor final evaluó la calidad de vida de los sujetos con DL con cuatro ítems.
Apéndice A
Discusión
El cuestionario de rendimiento orientado hacia los objetivos sobre la satisfacción de los fisioterapeutas basado la escala de Likert (goal-oriented performance Likert analysis questionnaire) de 32 ítems presentado en este estudio se utilizó para evaluar el grado de satisfacción del fisioterapeuta con la fisioterapia en sujetos con DL. El estudio discutió el procedimiento para elaborar el cuestionario. El objetivo principal de este cuestionario fue elaborar uno que contuviera todos los aspectos clínicos de la lumbalgia y valorase la satisfacción del fisioterapeuta mediante el logro de los objetivos, que pudiese utilizarse fácilmente en la investigación y en ámbitos clínicos.
Se observó que los niveles positivos de satisfacción de los fisioterapeutas y los pacientes están estrechamente asociados con cambios significativos y una mejoría en los síntomas clínicos. El concepto de elaborar un cuestionario de satisfacción del fisioterapeuta es dificultoso y multifactorial y no existen herramientas rápidas en las ciencias de la salud. La razón de esto puede deberse al hecho de que organizar en ítems altamente confiables y válidos los diversos signos y síntomas clínicos de DL es complejo.25,26
El cuestionario se elaboró con la fase inicial de encontrar los ítems correctos mediante diversos procedimientos y pruebas estadísticas.27,28 El autor prestó mucha atención a la descripción de los ítems en el cuestionario de una manera muy sensitiva, porque el participante puede negarse a expresar sus sentimientos originales algunas veces. Por lo tanto, todos los 32 ítems fueron analizados por el GIM y cada ítem proporcionó información sobre síntomas específicos. Las dos primeras fases del estudio se concentraron en la selección de ítems, que fue la fase más importante en la elaboración del cuestionario. El grupo de investigación realizó el análisis crítico y la revisión de los ítems para elaborar un cuestionario simple y preciso. Las palabras en el cuestionario fueron tales que podrían ser seguidas y entendidas por los fisioterapeutas con todos los grados y nivel educativo.
En la siguiente fase, se tuvieron en cuenta las sugerencias del fisioterapeuta con respecto a los ítems del cuestionario. Las respuestas individuales de todos los ítems de cada participante habían sido analizadas e incluidas en el cuestionario. Esto dio lugar a cambios significativos. El porcentaje de sesgo en este estudio se redujo al realizar diversos procedimientos analíticos en diferentes ámbitos de estudio con diferentes participantes.
Las pruebas estadísticas correctas se utilizaron para analizar su confiabilidad y validez y demostraron que podrían usarse en el DL para evaluar la satisfacción del fisioterapeuta. Se consideraron seis factores relacionados con los signos y síntomas clínicos de los pacientes para ser incluidos en el cuestionario. En nuestro estudio, todos los factores tuvieron puntajes de techo razonables, lo que demostró que este cuestionario es adecuado para encontrar el nivel de satisfacción en el enfoque de sujetos con DL. El cuestionario contenía 32 ítems que tenían una buena congruencia interna del coeficiente de Cronbach y la validez del cuestionario se probó con el método de análisis factorial.
El cuestionario se puede generalizar a todos los tipos de ámbitos clínicos porque durante la fase final del análisis de validez, y se envió a diferentes entornos. El cuestionario consistió en el componente de “calidad de vida” como el área más notable, lo cual es poco común en la mayoría de los cuestionarios de satisfacción. Luego, el efecto “halo” de la impresión común de algunos ítems y los ítems positivos y negativos en el cuestionario pueden afectar la respuesta y la dimensión del cuestionario. Todos estos factores podrían contribuir con la diversidad del cuestionario elaborado en el estudio.29-31
Algunos ítems del cuestionario se eliminaron del cuestionario inicial (Apéndice B) porque no cuadraron en las pruebas estadísticas, aunque a veces podrían ser útiles. El cuestionario no fue específico sobre la gravedad del DL, porque los signos y síntomas clínicos pueden variar según la gravedad.
Apéndice B
La validez externa del cuestionario no se analizó debido al hecho de que dichos cuestionarios estándar no estaban disponibles para medir la satisfacción del fisioterapeuta en los ámbitos clínicos. En los cuestionarios de medición subjetiva, a veces los participantes no responden como desean haber respondido.32 La tasa de respuesta del cuestionario fue inferior a lo esperado porque puede deberse a más ítems.
El Cuestionario de rendimiento orientado hacia los objetivos sobre la satisfacción de los fisioterapeutas basado la escala de Likert para determinar el grado de satisfacción del fisioterapeuta se probó con una variedad de pruebas estadísticas e indicó que el cuestionario era confiable y válido para determinar la satisfacción del fisioterapeuta con el tratamiento de las personas con DL.
|
 Bibliografía del artículo
Bibliografía del artículo
1. Mostagi FQ, Dias JM, Pereira LM, et al. Pilates versus general exercise effectiveness on pain and functionality in non-specific chronic low back pain subjects. J Bodyw Mov Ther 19:636-645, 2015.
2. Balagué F, Mannion AF, Pellisé F, et al. Non-specific low back pain. Lancet 379:482-91, 2012.
3. Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin 25:353-371, 2007.
4. Dagenais S, Tricco AC, Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine J 10:514-29, 2010.
5. Delitto A, George SZ, Van Dillen LR, et al. Low back pain. J Orthop Sports Phys Ther 42:A1-57, 2012.
6. Besen E, Young AE, Shaw WS. Returning to work following low back pain: towards a model of individual psychosocial factors. J Occup Rehabil 25:25-37, 2015.
7. Deyo RA, Bryan M, Comstock BA, et al. Trajectories of symptoms and function in older adults with low back disorders. Spine 40:1352-1362, 2015.
8. Minkalis AL, Vining RD. What is the pain source? A case report of a patient with low back pain and bilateral hip osteonecrosis. J Can Chiropr Assoc 59:300-310, 2015.
9. Van Middelkoop M, Rubinstein SM, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic nonspecific low back pain. Eur Spine J 20:19-39, 2011.
10. McCracken LM, Matthews AK, Tang TS, et al. A comparison of blacks and whites seeking treatment for chronic pain. Clin J Pain 17:249-255, 2001.
11. Portenoy RK, Ugarte C, Fuller I, et al. Population-based survey of pain in the United States: differences among white, African American, and Hispanic subjects. J Pain 5:317-328, 2004.
12. Ruehlman LS, Karoly P, Newton C. Comparing the experiential and psychosocial dimensions of chronic pain in African americans and Caucasians: findings from a national community sample. Pain Med 6:49-60, 2005.
13. Day MA, Thorn BE. The relationship of demographic and psychosocial variables to pain related outcomes in a rural chronic pain population. Pain 151:467-474, 2010.
14. Polsunas PJ, Sowa G, Fritz JM, et al. Deconstructing chronic low back pain in the older adult-step by step evidence and expert-based recommendations for evaluation and treatment: Part X: sacroiliac joint syndrome. Pain Med 17:1638-1647, 2016.
15. Airaksinen O, Brox JI, Cedraschi C, et al. COST B13 Working Group on Guidelines for Chronic Low Back Pain. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 15:192-300, 2006.
16. Chou R, Qaseem A, Snow V, et al. Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 147:478-491, 2007.
17. Carragee EJ, Hannibal M. Diagnostic evaluation of low back pain. Orthop Clin North Am 35:7-16, 2004.
18. Harris LE, Swindle RW, Mungai SM, et al. Measuring patient satisfaction for quality improvement. Med Care 37:1207-1213, 1999.
19. Roush SE, Sonstroem RJ. Development of the Physical Therapy Outpatient Satisfaction Survey (PTOPS). Phys Ther 79:159-170, 1999.
20. Goldstein MS, Elliott SD, Guccione AA. The development of an instrument to measure satisfaction with physical therapy. Phys Ther 80:853-863, 2000.
21. Nunnally JC, Bernstein IH. Psychometric theory. 3rd edition. New York, McGraw-Hill, 1994.
22. Raykov T, Marcoulides GA. Introduction to psychometric theory. New York, Routledge, 2011.
23. Spector PE, anonymous. Summated rating scale construction. In quantitative applications in the social sciences. London, SAGE, 1992.
24. Brace N, Kemp R, Snelgar R. SPSS for Psychologists. 3rd edition. London: Palgrave Macmillan, 2006.
25. Goossens ME, Vlaeyen JW, Hidding A, et al. Treatment expectancy affects the outcome of cognitive-behavioral interventions in chronic pain. Clin J Pain 21:18-26, 2005.
26. Romão AP, Gorayeb R, Romão GS, et al. High levels of anxiety and depression have a negative effect on quality of life of women with chronic pelvic pain. Int J Clin Pract 63:707-711, 2009.
27. Lipworth WL, Davey HM, Carter SM, et al. Beliefs and beyond: what can we learn from qualitative studies of lay people's understandings of cancer risk? Health Expect 13:113-124, 2010.
28. Gasquet I, Villeminot S, Estaquio C, et al. Construction of a questionnaire measuring outpatients' opinion of quality of hospital consultation departments. Health Qual Life Outcomes 2:2-43, 2004.
29. Roush SE, Sonstroem RJ. Development of the Physical Therapy Outpatient Satisfaction Survey (PTOPS). Phys Ther 79:159-170, 1999.
30. Goldstein MS, Elliott SD, Guccione AA. The development of an instrument to measure satisfaction with physical therapy. Phys Ther 80:853-863, 2000.
31. Oermann CM, Swank PR, Sockrider MM. Validation of an instrument measuring patient satisfaction with chest physiotherapy techniques in cystic fibrosis. Chest 118:92-97, 2000.
32. Wicker AW: Attitudes versus actions: the relationship of verbal and overt behavioral responses to attitude objects. J Soc Issues 25:41-78, 2010.
33. Etter JF, Perneger TV, Rougemont A. Does sponsorship matter in patient satisfaction surveys? A randomized trial. Med Care 34:327-335, 1996.
34. Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 46:1417-1432, 1993.
35. Stroh Wuolle K, Van Doren CL, Bryden AM, et al. Satisfaction with and usage of a handneuro prosthesis. Arch Phys Med Rehabil 80:206-213, 1999.
|
|